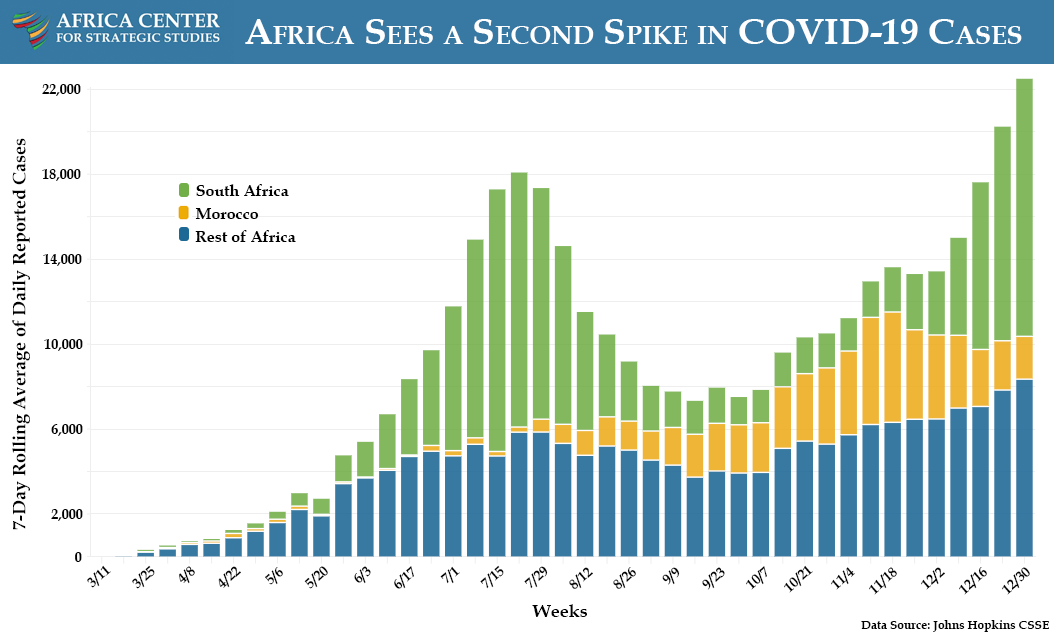
- An average of 28 of the continent’s 54 countries have reported a higher number of new COVID-19 cases each week compared to the previous week since the beginning of October. This trend has resulted in an average of 22,000 reported new cases per day in December, eclipsing the peak rate of 18,000 during the first wave in July. Nearly half of the total cases recorded on the continent have been reported since October.
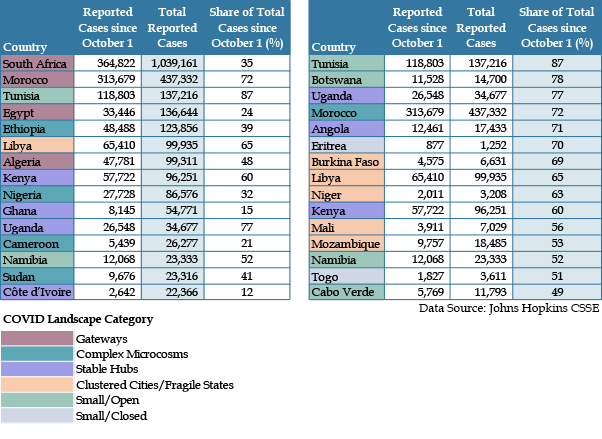
- Most recorded cases continue to be seen in South Africa and Morocco, which have among the best capacity for testing in Africa. Nonetheless, record levels of reported cases are observable continent-wide. Countries like Tunisia, Botswana, Uganda, Angola, Eritrea, and Burkina Faso, for example, have experienced steep increases in exposure during the second wave, though their cumulative number of reported cases remain relatively low.
- Mutations in the COVID-19 virus detected in South Africa and the United Kingdom (and potentially Nigeria) in December that make it significantly more transmissible raise prospects that the second wave could become even more dispersed. In South Africa, the mutated strain of the virus is dominant and driving the second wave. While the virulence of these new variants remains to be seen, it bears recalling that the second wave of the Spanish flu pandemic a century ago was more widespread and lethal in Africa (and other parts of the world) than the first.
- The surge may be particularly dangerous for public health systems in countries like Angola, Benin, Burkina Faso, the Democratic Republic of the Congo, Lesotho, Mali, Mauritania, Niger, Nigeria, and Togo, all of which have recorded their highest number of weekly cases during the second wave and whose public health systems were starting with fewer resources before the pandemic. Even countries with stronger health systems and those that are not yet experiencing surges during the second wave are still at risk of being overburdened as the virus spreads into rural or active conflict areas. In South Africa, the rising number of hospitalizations has required care to be rationed to those patients highest on triage lists.
- One of the striking characteristics of the first wave of the pandemic in Africa has been apparently lower mortality and morbidity than other parts of the world, perhaps because of the youthful demographics in much of the continent. Multiple studies suggest, however, that the asymptomatic spread of the disease has been significantly more widespread than these numbers might indicate. The emergence of new strains of the disease may then pose new dangers in countries where the combination of a more limited death toll but significant economic losses may make containment difficult. Other studies and reports indicate that significant numbers of COVID-19 fatalities may have been missed during the first wave in countries like South Africa, Sudan, and Nigeria.
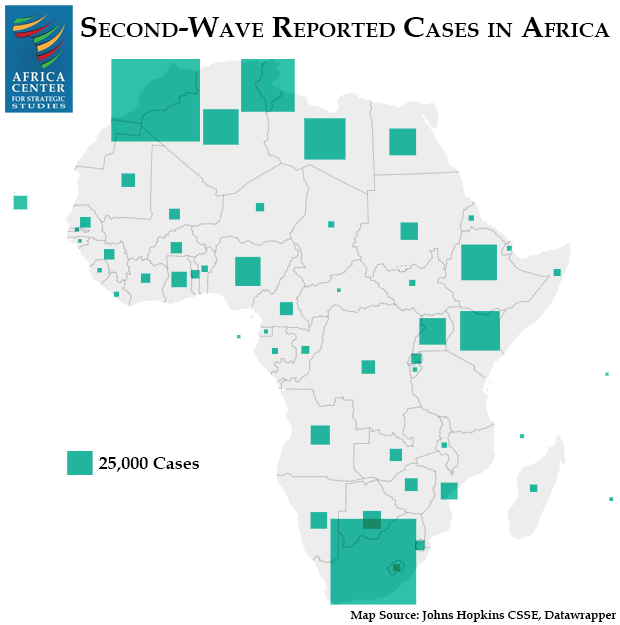
- Geographically, countries in North Africa and Southern Africa stand out in their reported exposure to this second wave (as well as testing). These nations also fit the typology of Gateway countries (i.e. those with significant international contacts) or those with large urban hubs.
- Many of the countries reporting a surge of cases in the second wave have high test positivity rates:
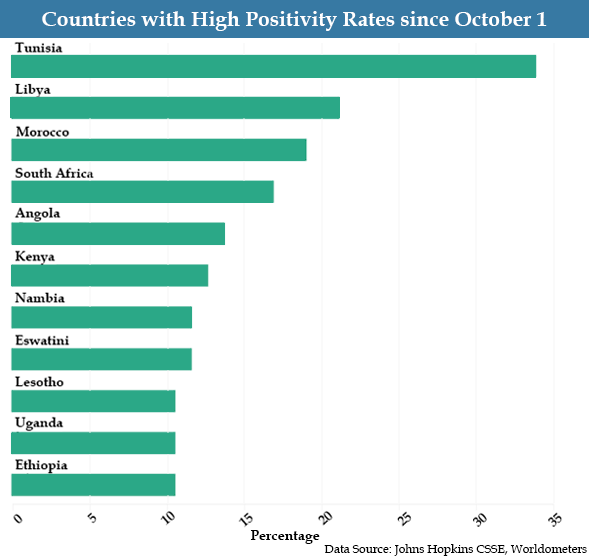
- This means the actual number of cases is likely much higher than is being captured by current levels of testing. This also suggests that countries with less extensive public health systems may be experiencing more cases than have been recorded. The Africa CDC is seeking more tests in addition to vaccines to more effectively control the virus. To date, ten African countries have conducted over 75 percent of the continent’s total recorded tests.
- While the second wave is spreading at a record pace across much of the continent, 93 percent of the recorded cases in the second wave are concentrated in 15 countries. For the continent as a whole, countries with relatively older populations, greater international exposure, and stronger public health systems to conduct testing have consistently reported higher numbers of cases. These 3 factors by themselves correlate with 55 percent of the second wave of reported cases.
- Aside from these factors, the prevalence of cases has varied greatly across the continent. Low levels of government transparency or democracy correlate to lower testing and case numbers, indicating that caseloads are likely further underreported in these countries. Tanzania stands out in this regard for its near absence of testing and reporting of cases. This opacity makes it difficult to know the true extent of the second wave and underscores the reality that a high number of reported cases is, in large part, a factor of testing capacity, clear public health communications, and transparency in publishing results.
- Shifts in the pattern of exposure can be seen during the second wave. Beyond the total number of reported cases, countries with sizable rural populations though large capital cities, such as in the Sahel, have experienced some of the most rapid rates of increase during the second wave. This suggests the virus is spreading beyond countries with significant international exposure. Many of these are also facing conflicts.
- Public health strategies of individual countries like Senegal, Nigeria, Ghana, and South Africa have mitigated the effects of the first wave. Likewise, the Africa Center for Disease Control (CDC) has coordinated with member states to establish the Africa Joint Continental Strategy for COVID-19, which has organized the continent’s monitoring, response, and communication on the state of the pandemic. Still, the pandemic’s disruptions and the enormous resources required to combat it have exacerbated fragility in many African countries. This fragility, combined with depleted public health systems as a result of the pandemic and public impressions that the virus is not afflicting average Africans, could make the second wave more threatening than the first.
- African public health officials are coordinating a massive and complex vaccination program. They are calling for full funding of the COVAX initiative to accelerate the timetable for inoculation across the continent. Without a successful vaccination program conducted in parallel with the rest of the world, the Africa CDC has warned that COVID-19 could become an endemic disease in Africa, creating an opportunity for the virus to mutate further, and slowing and complicating efforts to eradicate the virus globally.
Additional Resources
- Sheri Fink, “As Virus Resurges in Africa, Doctors Fear the Worst Is Yet to Come,” The New York Times, December 26, 2020.
- Africa Center for Strategic Studies, “Africa’s Varied COVID Landscapes,” Infographic, July 13, 2020.
- Africa Center for Strategic Studies, “Lessons from the 1918-1919 Spanish Flu Pandemic in Africa,” Spotlight, May 15, 2020.
- Africa Center for Strategic Studies, “Mapping Risk Factors for the Spread of COVID-19 in Africa,” Infographic, April 3, 2020.
- Africa Center for Strategic Studies, “Coronavirus Spreads through Africa,” Infographic, March 19, 2020 (updated weekly).
- Johns Hopkins University Center for Systems Science and Engineering COVID-19 Global Cases
- Africa Centres for Disease Control and Prevention
More on: COVID-19